Babies / Toddlers & Fever
Does your baby or toddler run a fever? We have some tips for you.
Help my baby/toddler has got fever!
Fever can have many causes:
Infections, but also increased physical activity raise the body temperature of the little ones. The increase in body temperature during infections is a protective reaction of the body. This is because it activates the body's defences and specifically fights pathogens by limiting their reproduction through the increased temperature. But how can I tell if I need to act and if my child is seriously ill? Because an elevated temperature during a growth spurt or teething is often a stressful phase for parents, but harmless for the child.
Which temperature is classified as fever?
So what are the limits for when a child has a fever? Normally, the body temperature is between 36.5° and 37.5° Celsius (between 97,7 and 99,5 Fahrenheit). Between 37.8 and 38.5° Celsius (between 100 and 101,3 Fahrenheit) the child has a raised temperature and from 38.6° Celsius (101,5 Fahrenheit) it is a fever. From 39.5° Celsius (103,1 Fahrenheit) the high fever begins. The temperature is usually highest in the evening.
How to take the temperature of my child / baby?
The rod thermometer can be used for 3 measuring methods.
- The oldest and most accurate method is to take the temperature in the anus (rectally). It is important to use a thermometer with a flexible tip. The measuring end is carefully inserted 1-2 cm into the anus. Depending on the device, the measurement takes between 10 and 30 seconds.
- You can also take the temperature in the mouth (oral/sublingual). This method can be inaccurate, especially if cold or hot food and drinks have been consumed in the last 10 minutes before the measurement. The measuring tip is carefully inserted into one of the two heat pockets under the tongue to the left or right of the root of the tongue. The mouth should be closed and the child should breathe through the nose. This method usually shows an inaccuracy of +/- 0.5 °C.
- You can also use a rod thermometer to measure under the arm (axillary). Here, too, there are measurement inaccuracies. The temperature is usually measured a little too low. The skin must be dry and the measuring tip is placed under the arm so that there is good skin contact. The thermometer is placed at a right angle to the body and the child's arm is best placed over the chest so that the thermometer is tight. This is usually 0.5°C too low.
Please remember to clean the thermometer before and after each use. A protective cover is a practical addition.
There are also ear thermometers. Here you have to make sure that the ear of children over 1 year is pulled slightly upwards/backwards in the middle. This allows more skin contact for the measurement and a more accurate result. For children under one year of age, only pull the auricle back a little. While gently pulling the ear, the measurement sensor is inserted and the measurement is taken. Most devices have a signal tone when the measurement has been taken. (approx. 1-3 seconds)
Another method is the forehead measurement. The forehead thermometer is held in front of the forehead, a maximum of 3 cm from the centre of the forehead. The measuring sensor is directed between the eyebrows. The forehead must not be covered with hair, sweat or dirt. If the measuring points have just been cleaned by friction, you should wait for a few minutes until the measurement is taken, otherwise the measurements could be falsified. During the measurement, it is important that the thermometer is held still and that the child is also calm, otherwise the measurement result may be affected.
With all methods, it is important to look for a CE test seal and to read the operating instructions carefully.
As a personal tip, I can say that I always have a rod thermometer with a flexible tip and an ear thermometer at home. If I only want to check the temperature briefly, I use the ear thermometer (also good for us adults) because it measures well and the whole thing works very quickly. However, I am aware of a certain measurement inaccuracy and always have a stick thermometer at home for emergencies. In the first year, I only measured my children's rectal temperature with a stick thermometer.
But what should I do if my child has fever?
If you have an infant of less three months of age, always go to the doctor or ER if the temperature is above 37,8 degree.
First of all, observe your child.
The general recommendation is to go to the pediatrician, if the fever is above 38 degrees and you are not yet sure how your baby reacts (and also you) towards fever.
If he or she is listless, unresponsive and not drinking enough, you should definitely consult a doctor.
If a child has a temperature below 39 degrees Celsius 102,2 Fahrenheit) , you do not necessarily have to give fever-reducing medication. Just see how your child feels and whether he or she is suffering from the temperature. Fever is a natural reaction of the body to fighting and therefore also to be seen as a natural defence mechanism.
From 39.0 ° Celsius, a fever-reducing measure can makes sense, but is not a must.
First of all, if your child has a fever, he or she should drink a lot (tea, diluted fruit juice, water), preferably something every few minutes. Smaller portions but continuously would be optimal.
In addition, the child/baby should not be dressed too thickly or have too many blankets. This is not recommended for babies with regard to SID and it also contributes to overheating. Clothing adapted to the outside temperature is best.
- To reduce the child's fever somewhat, you can use calf wraps (but only if the hand/feet are warm!). Fold a cotton or linen cloth several times lengthwise and dip the cloth in warm (NOT COLD) water (approx. 30° C, 86 Fahrenheit). It should not drip and should be wrung out. Now wrap the lukewarm cloth around the lower legs. Please make sure that the cloth is not too loose, otherwise the wraps will not work. Then an outer cloth is wrapped around the lower leg. After 15 minutes, the cloths are removed. You should not make a wrap more than once an hour. During the rise in fever, children feel cold and shiver. At this time, a calf wrap is not appropriate. Also the feet of your child needs to be warm to do the wraps.
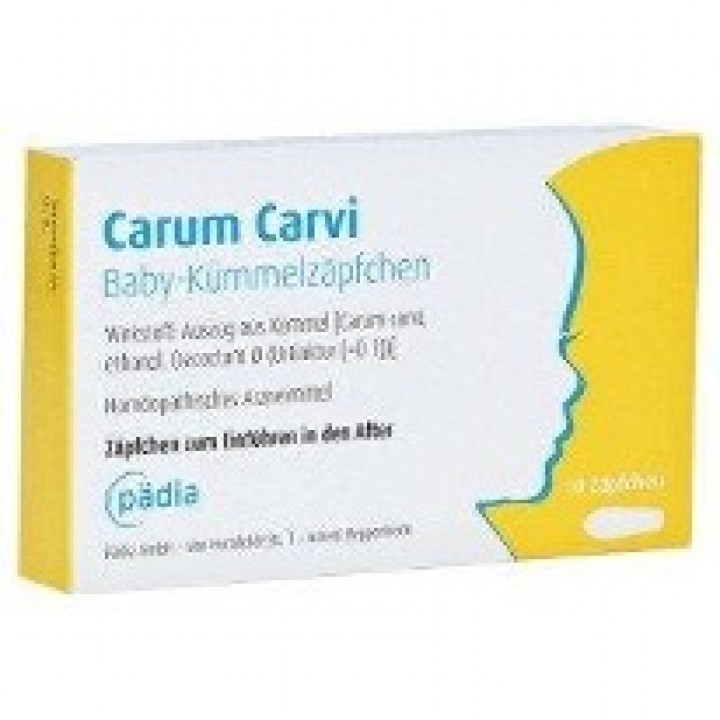
- Of course, you can also use fever juice and suppositories to reduce fever. Some fever medicines also have analgesic and anti-inflammatory properties. Please always observe the special dosages for babies and small children. These can also be found in the package leaflet. From the age of about 1 year, a fibre juice is most likely to be used, before that suppositories. From about 6-8 years, the first tablets are also available. Normally, the medicines take effect within 30 minutes. Please note the maximum dose of the medication. Paracetamol in particular can have serious side effects if taken in excess.
Please always ask at the pharmacy or your paediatrician.
Can there be complications?
In rare cases, a febrile convulsion can occur. This is a seizure that occurs in children during a febrile infection. It is usually triggered by a sudden, rapid rise in fever. Children between six months and six years are particularly at risk. These convulsions are often mistaken for epilepsy. However, they are very rarely associated with this disease.
The children roll their eyes, do not react and stare into space. Sometimes they even pass out and get blue lips. Twitching may occur. Usually, such a seizure is over after less than a minute. Normally, a febrile seizure has no permanent consequences.
Call the ambulance immediately on 112 if this is the first seizure or if it lasts longer. There is a risk of hypoxia or even cardiovascular arrest. It is important to get the child into a safe position so that it cannot injure itself or fall down somewhere.
When the seizure is over, the child can be placed in a stable lateral position and care should be taken to ensure that the airway is clear. If the child is not breathing, resuscitation should be started. However, this is extremely rare.
Once your child had a seizure you will get emergency medication for him/her to take in case this happens again, which is also extremely rare.
The doctor is also the right person to talk to if your child has been ill for more than 3 days and has a fever well above 39°C, or if a skin rash or other symptoms occur. And as mentioned above, keep an eye on your child. If your child is listless, does not drink enough and can hardly be woken up, you should definitely consult a doctor.
Also if you are not sure and feel insecure, please always consult your doctor.
The following pictures contains only examples of medications. This is not an advertisement, just a personal recommendation. There are different manufacturers of the different medication groups.
For more information, please contact your pharmacy or doctor.
Juli 2021 - Gravidamiga
This blog post has been prepared with the greatest possible care and does not claim to be correct, complete or up-to-date.“ This is not a medical post and it does NOT substitute a visit to a doctor.
Tell someone of us today - thank you!
https://www.instagram.com/gravidamiga/
https://www.facebook.com/gravidamiga
and sign up for our weekly Gravidamiga Newsletter.
or check out our partner page for more general information about life in Stuttgart with an extensive blog:
Kiramiga - beyond relocation.
We love what we do and hope you love it, too.
Please support us and our work by donating us a coffee or a prosecco :-)
Thank you.
Updated: August 2022
Posted in in Babies & Toddlers, Medicine & Psychology